TIM-3 Alzheimer’s therapy represents a groundbreaking approach in the fight against Alzheimer’s disease, leveraging insights from the immune system to tackle the challenges posed by this neurodegenerative disorder. Recent studies suggest that targeting the TIM-3 checkpoint molecule, which inhibits microglia—the brain’s immune cells—could enhance their ability to clear amyloid plaques, a hallmark of Alzheimer’s. By reactivating microglial function, researchers have demonstrated significant improvements in cognitive performance in mice, raising hopes for effective Alzheimer’s disease treatment strategies. As ongoing research bridges the gap between cancer immunotherapy and neurodegenerative disease research, TIM-3 could be pivotal in reshaping our understanding of immune system and Alzheimer’s interactions. Given that late-onset Alzheimer’s accounts for the majority of cases, this innovative therapy could be a key to unlocking new avenues for prevention and management.
The therapy targeting TIM-3 in Alzheimer’s disease brings a fresh perspective to the treatment of age-related cognitive decline. By inhibiting the function of a specific checkpoint molecule, this approach aims to revitalize the brain’s immune response, specifically enhancing the role of microglia in clearing harmful plaques. This line of research parallels advances in cancer immunotherapy, where similar strategies have yielded promising results, suggesting a possible crossover in therapeutic applications. Researchers are increasingly recognizing the importance of the immune system’s regulation in combating neurodegenerative conditions, while also exploring innovative methodologies that might transform Alzheimer’s disease treatment. With significant findings emerging, the future holds potential for novel interventions that harness the body’s own defenses to restore cognitive health.
Exploring TIM-3 as a Potential Alzheimer’s Therapy
Recent studies indicate that TIM-3, an immune checkpoint molecule, could play a transformative role in the treatment of Alzheimer’s disease. Researchers have discovered that by deleting TIM-3 in mouse models of late-onset Alzheimer’s, microglia, the brain’s immune cells, were freed to attack and clear amyloid plaques. These findings suggest that TIM-3 not only serves as an inhibitor of immune response but also represents a novel therapeutic target in the fight against neurodegenerative diseases, indicating a promising direction for future treatments.
The implications of utilizing TIM-3 Alzheimer’s therapy extend beyond just improving cognition in mice. If successful in human trials, such therapies could pave the way for more effective treatments following years of disappointing drug trials in Alzheimer’s research. The potential to repurpose existing anti-TIM-3 antibodies may also expedite the strategy towards clinical applications, propelling this avenue of treatment forward in response to Alzheimer’s relentless progression.
The Role of Microglia in Alzheimer’s Disease
Microglia are essential players in brain health, acting as the first line of defense against pathogens and brain debris. In the context of Alzheimer’s disease, however, these immune cells exhibit altered behavior, often failing to clear amyloid plaques effectively. The increased expression of checkpoint molecules like TIM-3 on microglia hampers their ability to engulf harmful plaque, leading to the accumulation of debris that exacerbates neurodegeneration. This maladaptive response underscores the importance of microglia in understanding and addressing Alzheimer’s disease.
Research highlighted in recent studies points to a significant relationship between microglial activity, TIM-3 expression, and Alzheimer’s pathology. As these cells adapt to maintain homeostasis, they become less effective at their crucial clearing functions, which is critical in a condition characterized by plaque buildup. By targeting TIM-3, therapies aiming to reinvigorate microglial functions could hold the key to reversing some of the cognitive declines associated with Alzheimer’s disease.
Cancer Immunotherapy Strategies Inform Alzheimer’s Research
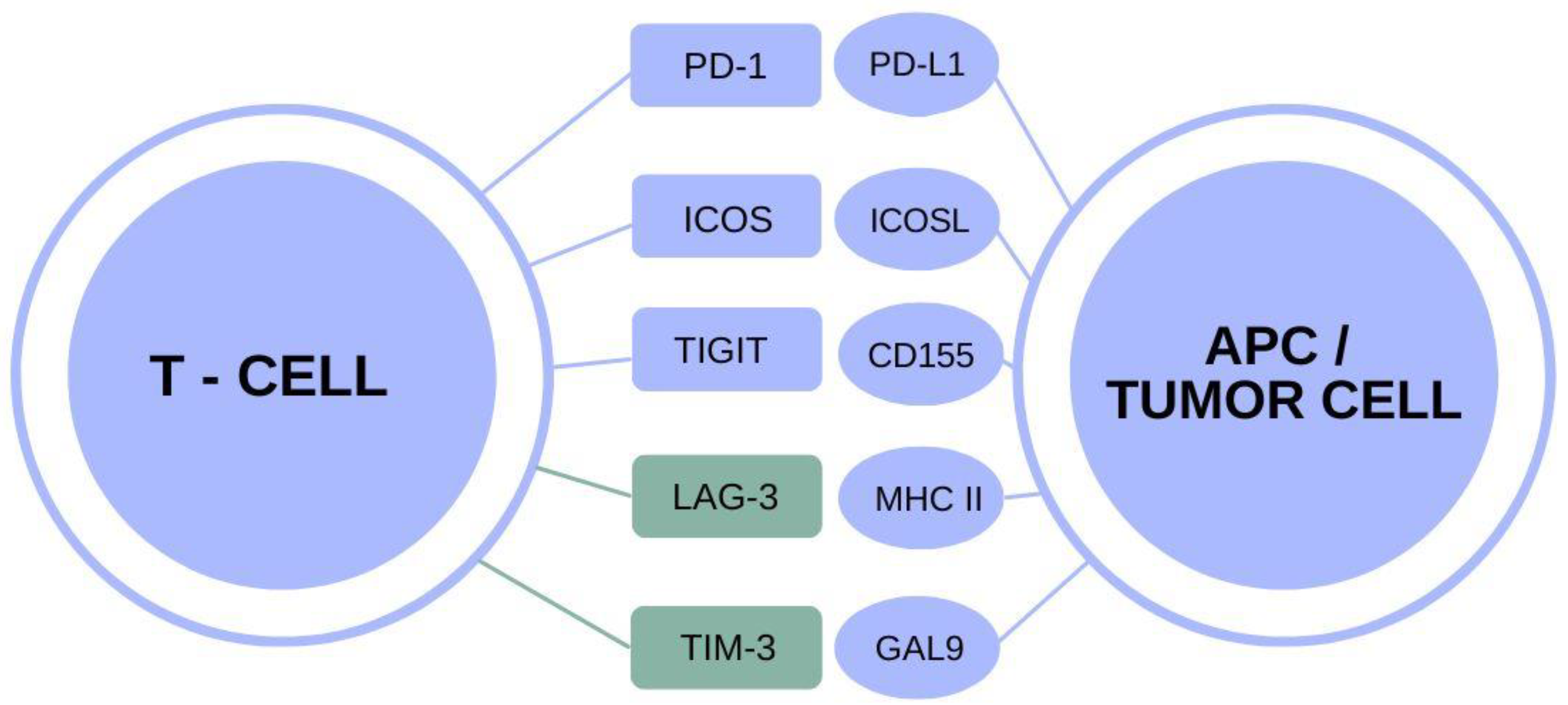
The parallels between cancer immunotherapy and Alzheimer’s disease treatment open up exciting possibilities for research and treatment strategies. Cancer treatments that leverage checkpoint inhibitors, such as TIM-3, provide a framework for understanding how similar techniques could be adapted for neurodegenerative diseases. Both conditions involve the regulation of immune responses; therefore, insights from cancer immunotherapy can inspire innovative approaches to modulating microglial activity in Alzheimer’s disease.
Such similarities suggest a potential pipeline for developing TIM-3 Alzheimer’s therapy drawn from established cancer treatments. Science has shown that inhibiting checkpoint molecules can rejuvenate immune responses in cancer, and similar approaches may help restore the capability of microglia in the context of Alzheimer’s. As research evolves, the integration of concepts from diverse fields could accelerate the onset of viable therapies for neurodegenerative diseases.
Understanding the Genetic Factors of Alzheimer’s Disease
Genetic components significantly shape the risk and response to Alzheimer’s disease, with TIM-3 emerging as a notable candidate linked to late-onset forms of the illness. Variants in the HAVCR2 gene, which encodes TIM-3, have been associated with increased susceptibility to Alzheimer’s, indicating that inflammatory pathways may contribute to disease pathology. Uncovering these genetic links can lead to targeted therapies that take personal genetics into account, enhancing treatment efficacy.
The focus on genetic predisposition, particularly regarding TIM-3, highlights the need for precision medicine in Alzheimer’s research. Tailoring therapies based on genetic profiles not only opens the door for more effective treatment options but also enhances our understanding of how immune responses can be modulated in these patients. Thus, exploring the genetics of Alzheimer’s and its relationship with TIM-3 is vital for advancing both research and therapeutic developments.
The Mechanism of Microglial Dysfunction in Alzheimer’s
Microglial dysfunction plays a critical role in the pathogenesis of Alzheimer’s disease, particularly through the lens of TIM-3 involvement. As immune cells of the brain, microglia are tasked with clearing amyloid plaques and dead neurons but become increasingly ineffective as Alzheimer’s progresses. This dysfunction is attributed to TIM-3’s overexpression, which inhibits microglial activation and impairs their phagocytic abilities, essential for brain health.
This understanding of microglial dysfunction suggests that reversing TIM-3 activity could restore microglial function, allowing them to fulfill their role in plaque clearance. By reinvigorating this immune response, potential therapies could not only reduce amyloid burdens but also improve cognitive outcomes, representing a significant leap forward in Alzheimer’s disease treatment strategies.
Potential Advances in Alzheimer’s Therapeutics through TIM-3
The promising interactions between TIM-3 and Alzheimer’s therapy suggest an innovative frontier in the treatment landscape. By focusing on how TIM-3 inhibits essential microglial functions, researchers have identified a potential target for therapeutic intervention that stands to alleviate the cognitive decline associated with Alzheimer’s. The approach of utilizing TIM-3 inhibitors could lead to significant breakthroughs in restoring immune functions disrupted in Alzheimer’s pathology.
Aside from targeting plaques, TIM-3 Alzheimer’s therapy could have broader implications by enhancing synaptic function and overall brain health. This multifaceted potential for TIM-3 strategies reflects the intricate relationship between the immune system and neurodegenerative disease, setting the stage for future exploratory studies and eventual clinical applications aimed at improving life quality for Alzheimer’s patients.
Challenges in Targeting TIM-3 for Alzheimer’s Treatment
While targeting TIM-3 for Alzheimer’s treatment presents significant promise, important challenges remain to be addressed. One major consideration is the need for selective targeting that avoids compromising normal immune function in the brain, as TIM-3 plays a vital role in regulating microglial activity. Careful pharmacological design is essential to ensure that interventions enhance microglial plaque clearance without inadvertently leading to overactivation that could cause harm.
Moreover, translating preclinical successes observed in mouse models to human patients requires rigorous testing to ascertain safety and therapeutic effectiveness. The journey from innovation in the lab to real-world application involves navigating regulatory landscapes and addressing efficacy in the complexity of human biology, particularly in a disease as enigmatic as Alzheimer’s.
Future Directions in Alzheimer’s Research with TIM-3
The investigation into TIM-3 as a therapeutic target opens up numerous future directions for Alzheimer’s research. Studies are currently exploring the efficacy of TIM-3 inhibitors in various model systems, and ongoing research aims to monitor their impact in humanized models designed to mimic Alzheimer’s pathology accurately. Moreover, as we learn more about TIM-3’s multifaceted roles in immune regulation, our understanding of its influence may expand beyond Alzheimer’s to other neurodegenerative conditions.
Looking ahead, collaborative efforts integrating insights from diverse fields — such as immunology, genetics, and neurology — will be crucial in advancing TIM-3 Alzheimer’s therapy into clinical practice. By building on the foundations of this research, scientists aim to revolutionize conventional approaches to Alzheimer’s treatment and potentially alter the disease course, offering hope for future generations afflicted by this devastating condition.
The Importance of Biomarkers in Alzheimer’s Research
Biomarkers are essential tools in Alzheimer’s research, providing vital information about the presence and progression of the disease. In collaboration with strategies involving TIM-3, developing reliable biomarkers can help monitor therapeutic effectiveness and disease modification. The identification of specific biomarkers related to TIM-3 activity might enhance diagnostic accuracy and pave the way for personalized treatment approaches.
As researchers explore the dynamics between biomarkers, TIM-3 levels, and microglial functions, a clearer picture of the disease’s pathology will emerge. This could lead to earlier interventions, improved patient stratification for trials, and better outcomes for individuals suffering from Alzheimer’s. Thus, biomarkers are not just informative but are integral to shaping the future landscape of Alzheimer’s treatment.
Frequently Asked Questions
What is TIM-3 Alzheimer’s therapy?
TIM-3 Alzheimer’s therapy refers to a novel treatment approach that targets the TIM-3 molecule in the brain’s immune cells, known as microglia, to enhance their ability to clear amyloid plaques associated with Alzheimer’s disease. This strategy is inspired by cancer immunotherapy, which uses similar checkpoint inhibitors to activate the immune system against tumors.
How does TIM-3 affect microglia in Alzheimer’s disease?
In Alzheimer’s disease, the TIM-3 molecule inhibits microglia from attacking and clearing amyloid plaques. High levels of TIM-3 lead to a state called homeostasis in microglia, preventing them from engaging in phagocytosis and contributing to plaque clearance, which is crucial for cognitive health.
Can TIM-3 Alzheimer’s therapy improve cognition in patients?
While TIM-3 Alzheimer’s therapy has shown promise in mouse models, where cognitive functions improved after TIM-3 was blocked, clinical trials are needed to determine its effectiveness in human patients suffering from Alzheimer’s disease. The goal is to repurpose existing anti-TIM-3 antibodies to enhance memory and cognitive function.
What are the potential benefits of targeting TIM-3 in Alzheimer’s treatment?
Targeting TIM-3 in Alzheimer’s treatment could potentially reverse some cognitive deficits by enhancing the ability of microglia to clear amyloid plaques. This approach could address a major challenge in Alzheimer’s therapy, as traditional treatments have often failed to effectively clear these neurotoxic plaques.
How does TIM-3 relate to the immune system and Alzheimer’s disease?
TIM-3 is a checkpoint molecule that plays a significant role in regulating the immune response. In Alzheimer’s disease, the excessive expression of TIM-3 on microglia hampers their ability to clear amyloid plaques, leading to increased neurodegeneration and cognitive decline.
What research has been conducted on TIM-3 and Alzheimer’s disease?
Recent research has demonstrated that deleting the TIM-3 gene in mouse models leads to improved plaque clearance and cognitive function recovery. This research highlights the therapeutic potential of TIM-3 inhibition in treating Alzheimer’s disease, aligning with concepts from cancer immunotherapy.
Are there any clinical trials for TIM-3 Alzheimer’s therapy?
As of now, clinical trials specifically targeting TIM-3 for Alzheimer’s treatment are in early stages. Researchers are optimistic as preliminary findings have shown that anti-TIM-3 therapies may halt the progression of amyloid plaques in models that simulate human Alzheimer’s disease.
What challenges does TIM-3 therapy face in Alzheimer’s research?
Challenges include achieving effective delivery of anti-TIM-3 therapies to the brain, ensuring safety and efficacy in the human population, and overcoming the historical difficulties associated with Alzheimer’s drug development, where many treatments have failed in clinical trials.
What is the significance of TIM-3 as a genetic risk factor for Alzheimer’s?
The TIM-3 gene has been identified as a genetic risk factor for late-onset Alzheimer’s disease, with specific polymorphisms linked to higher TIM-3 expression levels. Understanding this relationship could enhance prevention strategies and therapeutic interventions aimed at modulating the immune response in Alzheimer’s patients.
Could TIM-3 Alzheimer’s therapy also benefit other neurodegenerative diseases?
While TIM-3 Alzheimer’s therapy primarily targets amyloid plaques in Alzheimer’s disease, its mechanisms could potentially be explored for other neurodegenerative diseases where similar immune dysfunctions are observed, highlighting the broader implications of TIM-3 modulation in neurodegenerative disease research.
| Key Points | Description |
|---|---|
| Study Overview | A study suggests that a cancer treatment strategy may also help Alzheimer’s disease by targeting the TIM-3 molecule. |
| Immune System Insights | TIM-3 is an immune checkpoint molecule that inhibits microglia from clearing amyloid plaques in the brain. |
| Alzheimer’s Prevalence | 90-95% of Alzheimer’s cases are late-onset, associated with genetic factors related to TIM-3. |
| Microglia Functions | Microglia are immunological cells that prune synapses and clear plaques; TIM-3 inhibition affects their activity. |
| Therapeutic Potential | Blocking TIM-3 may enhance plaque clearance and improve cognition in Alzheimer’s disease models. |
| Future Directions | Research is ongoing to test anti-TIM-3 therapies on humanized mouse models of Alzheimer’s. |
Summary
TIM-3 Alzheimer’s therapy offers a promising avenue for combating Alzheimer’s disease by leveraging immune system strategies previously successful in cancer treatments. As research continues to explore the impact of inhibiting the TIM-3 molecule, there is hope for significant advancements in memory restoration and plaque clearance mechanisms in the brain. This innovative approach might transform treatment strategies for Alzheimer’s, providing new hope for those affected by this debilitating condition.